Technological advancement is one of the core parts of the development of radiotherapy, much in the same way that radiation therapy is one of the core parts of the treatment of many lesions, tumours and types of cancer.
Because of this, radiotherapy tends to be one of the most unique and fast-moving fields of research in all of medicine, as each revolutionary change serves to make treatments that were previously impossible almost routine in their effectiveness.
One of the most interesting recent developments is in the field of Biology-Guided Radiotherapy (BgRT), a promising emerging field of radiotherapy that allows for more adaptive treatments and avoids overly cautious treatment plans that might make certain tumours inoperable due to unacceptable levels of risk.
At this early stage, only a few treatment centres are using BgRT, but as the concept increases in its capabilities and more radiotherapy centres look to adopt the most state-of-the-art technological advances, here is everything you need to know about this new field.
What Is Biology-Guided Radiotherapy?
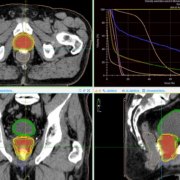
The core principle behind BgRT is that it combines radiotherapy treatments with positron emission tomography (PET), a system that creates digitised, detailed imagery of the body as it is currently functioning, rather than a static two-dimensional or three-dimensional model of how it looks.
It works through the use of a radiotracer, which is injected into the bloodstream and through tracking the activity of this radioactive substance in real-time, can also track the exact position of cancerous cells at a given time.
PET is often used in conjunction with CT scans for more accurate readings, but in radiotherapy, it delivers something potentially far greater and something that can unlock a very powerful treatment that it would be impossible to use otherwise.
How Would It Change Treatments?
At present, radiotherapy is undertaken through the use of a static body scan (typically a CT scan) that is used to coordinate and prepare the treatment, as well as explore what exact options are available.
The problem with a static scan is that whilst the scan itself is accurate and detailed and static, the human body it is depicting is very much not, and various organs and parts of the body can shift and change position in the body, both naturally and as a process of movement.
This means that where the tumour was when the CT scan was made days or even weeks before, and where it is when the radiotherapy treatment takes place can be very different indeed, and in order to compensate for this, radiotherapy treatments tend to be broader than they perhaps need to be.
Because there is the potential for collateral harm, radiotherapy is often best used with smaller tumours, and is often combined with chemotherapy or other forms of cancer medication to shrink the tumour and make it far easier to destroy without damaging too much healthy tissue.
The best way to undertake radiotherapy, therefore, would be to combine it with a real-time diagnostic imaging system, as there would be no difference between the scan and the body that was being treated and this would lead to radically more accurate treatments.
There are a lot of ways to do this potentially, with explorations into using real-time CT scans and even modified forms of ultrasound, but the one with the most potential is BgRT, because of the inherent real-time nature of how PET interacts with cancer cells.
Cancer tends to be particularly easy to spot with PET, and even if it moves, it is very clear to see where it is at any given point, allowing for rapid adaptation to tumours that are moving around the body.
This not only leads to more accurate treatment and faster recovery times for treating tumours and growths that are already managed through other more conventional forms of treatment, but also allows for more complex cancers to be treated.
In particular, treating multiple tumours is a complex process that requires each tumour to be treated individually, with a separate CT scan and planning process for each.
This novel BgRT approach allows for several tumours to be treated at once, helping to reduce overall treatment times and ensure there are fewer complications.
It also allows for subtle patient movements to be factored in, which means that patients do not necessarily have to be held completely still in order for a treatment to be effective.
It could potentially mean that tumours too close to vital organs to be viably operable up to this point could be treatable in the near future.