There are many causes of chronic pain and, as a result, there is a broad range of different treatment types that can provide a lifeline to some people living with pain symptoms.
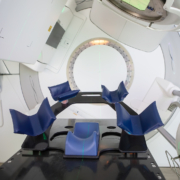
One of these is low-dose radiotherapy, which is particularly effective at helping alleviate musculoskeletal pain very quickly and very effectively.
Unlike radiotherapy for cancer care, these radiotherapy sessions are typically undertaken either as required or on an occasional basis, take a matter of seconds to complete and are entirely non-invasive.
Many people are likely to start feeling the benefits before the treatment course is over and continue to enjoy a pain-free life for a long time afterwards, but because chronic pain has many different causes, the journey to recovery can look and feel different for different people.
One aspect of this is that some people will feel better and recover as the radiotherapy course is taking place, but others will notice a more intense spike in pain that gets better and leads to a less painful baseline.
Despite being very different sensations, they often both signify a road to recovery, but to understand why, we need to explore chronic pain, its causes and why radiotherapy can help in the first place.
What Is Pain?
Defining pain is both extremely easy and almost impossible, because whilst we intuitively know that pain hurts, we all feel pain differently and pain episodes will sometimes feel different to each other even if they have the same cause.
This is because pain is best defined as a biopsychosocial phenomenon; pain is not only caused by biological phenomena such as injury or tissue damage but is also caused or intensified by psychological factors and environmental conditions.
The British Pain Society notes that whilst acute pain is typically a warning signal to highlight that a body part is hurt or an infection is making you ill, chronic and intermittent pain often has no useful purpose and can be caused by a wide range of factors affecting nerve signals.
Pain is often situational, which is why people in a flight-or-fight situation may not feel pain when they are in that crisis situation even if they feel it afterwards.
When Can Low-Dose Radiotherapy Help Chronic Pain?
Chronic pain has a wide variety of causes and a major part of pain management and treatment is working out the root cause of chronic pain. Some of these causes can be effectively treated through radiotherapy, especially if medication and physiotherapy have proven to be ineffective.
One condition that radiotherapy has proven to be effective at treating is osteoarthritis, one of the most common chronic pain disorders in the world.
Recent research into the causes of arthritis symptoms notes the effect of inflammation on the progression and pain of the disease, and the anti-inflammatory nature of low-dose radiation makes it an ideal non-invasive treatment that has proven to be effective for many people.
It can also help with other, similar conditions involving soft tissue pain such as plantar fasciitis, as well as treating chronic pain and swelling around the joints, something that not only relieves pain but can improve range of motion as well as quality of life.
Finally, radiotherapy can sometimes be used palliatively in order to relieve the pressure and symptoms of a cancerous tumour by shrinking it, usually when it is considered to be otherwise inoperable.
Can Low-Dose Radiotherapy Cause Pain?
In the overwhelming majority of cases, radiotherapy is instant, painless and the effects can be felt very quickly, due to the targeted nature of the radiation used.
However, there are a few very rare cases where a chronic pain relief treatment can cause pain to increase as a sign that it is effectively treating the condition causing chronic pain.
The principle is similar to delayed onset muscle soreness (DOMS), the pain felt following a workout that is typically caused by the same microscopic tears to muscles and ligaments that lead to muscle growth.
In some cases, chronic pain recovery is about activating parts of the body’s recovery and recuperative systems to restore function and lead to long-term benefits.
In those cases, and a doctor will let you know if that is likely to be the case, the pain is a sign that the joint, soft tissue or other area in the body is effectively responding to treatment. The pain will go away, and it will often lead to significant relief in chronic pain.
This is not always the case, and if you do not feel a spike in pain but do feel pain relief of chronic symptoms, that is just as effective a sign of recovery.