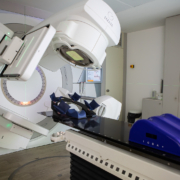
Anyone who is prescribed a course of radiotherapy treatments from a specialist centre can feel comforted that they are receiving a proven treatment that is over a century old and is still evolving and improving in its efficacy.
From the very start of radiotherapy’s development as a potential treatment for cancer, the effectiveness of radiation was never in doubt, because the underlying therapeutic principle largely predates the discovery of radiation itself.
Replacing Chemicals And Electricity
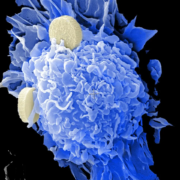
The therapeutic action of radiotherapy is to burn away the tissue that is exposed to radiation, which means that its targeted use can effectively destroy unwanted cells.
The main developments from this discovery in 1896 by Leopold Freund, Eduard Schiff, Emil Grubbe and Victor Despeignes paved the way for progressively better targeted, safer and more effective forms of treatment.
However, the underlying therapeutic action was much older than this, even if the tools used to destroy the malignant tissue were far less accurate and far more dangerous.
Early 1800s: Electrotherapy
One main form of treatment which inspired the development of radiotherapy once radiation was discovered was electrotherapy.
Unlike modern electrotherapy, which tends to use small electrical currents to stimulate recovery or enhance the effects of certain chemotherapy treatments, the field of electrotherapy up until the early 19th century was rather more experimental.
Up until Golding Bird, who helped rehabilitate the field of electrotherapy in the same way that Henri Coutard would radiotherapy in the 1930s, electrotherapy was another treatment that was often extremely dangerous with somewhat dubious benefits.
It was used to stimulate skin tissue and potentially burn away unwanted cancerous cells, and this method of action still sees some use today in the treatment of varicose veins.
Early 1900s: Escharotics
One of the earliest forms of treatment for killing unwanted tissue was poisonous and caustic substances called escharotics. However, these substances are not only extremely dangerous, scarring and in some cases outright mutilating, they can cause permanent, potentially life-threatening damage.
They were popular in early medical practice up until the early 1900s because, without the knowledge of how tumours survive, the tumour did appear to be burned away, along with a significant chunk of healthy tissue, making it appear to be effective even if the tumour very often grew back.
Escharotics have been largely discredited by mainstream medical practice since, and many of the substances used are illegal to sell because of the significant amounts of damage they can cause.
Even the few forms of cancer that can be treated topically such as basal cell carcinoma are typically treated with less damaging and more effective topical solutions than caustic chemical burns.
1896: Discovery of radiation
As early as 1896, doctors knew that radiation could provide the same ablative effect, even if they did not quite understand why.
Victor Despeignes accidentally discovered the therapeutic effects of radiotherapy when trying to treat a patient with late-stage stomach cancer.
Whilst he ultimately did not survive and Mr Despeignes only opted for radiotherapy under the mistaken belief that cancer was caused by parasites, it inadvertently proved a principle that would be more effectively demonstrated by Mr Freund and Mr Schiff, and mark a seismic shift in the history of medicine.
1933: Stereotactic frame & electrotherapy
Interestingly, the first use of the stereotactic frame to treat a human patient involved electrotherapy.
In 1933, Martin Kirschner published a paper wherein he detailed his use of a treatment for trigeminal neuralgia by using a stereotactic frame to make an incision large enough to feed an electrode to the trigeminal nerve, burning it away and reducing the pain.
1940s: Gamma Knife development
This principle would later be used by Lars Leksell for his innovative Gamma Knife radiosurgery and serves to highlight just how influential pre-radiation radiotherapy treatments were and how similar their core method of action is.
The main difference, of course, is a matter of scale, effect and invasiveness to a patient.
Surgery was and remains very effective but is also extremely invasive and typically requires a patient to spend several nights in the hospital to recover.
Escharotics may not require incisions but they are invasive and require time to recover from the intense and often unpredictable damage that the materials could cause. This lack of consistency is what led to them being almost universally outlawed.
Electrotherapy was less invasive but in some cases still required an actual incision to provide the same effect of ablation and burning away of unwanted or harmful tissue.
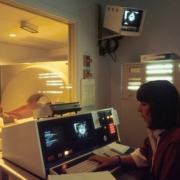
2025: AI in radiotherapy
In early January 2025, researchers explored the potential of using AI to make what had become an already accurate set of treatments even more precise, something that has some benefits for brain lesions and tumours but can be even more important for treating cancers that affect the digestive and reproductive systems.